Non Alcoholic Fatty Liver vs Alcoholic Fatty Liver: Causes & Treatment

In India, it’s no longer unusual to hear a doctor warn even a young, non-drinking individual: “Your liver looks fatty.” That raises a natural question: how can someone who has never touched alcohol end up with a fatty liver?
Honestly, fatty liver is no longer merely an "alcoholic’s disease." Numerous lifestyle changes, such as diets, inactivity, stress, and the intake of processed foods, have led to liver issues that are significantly prevalent to both drinkers and non-drinkers. The Indian National Association for the Study of the Liver (INASL) estimates that about one-third of people residing in cities of India may be living with a fatty liver without being aware of it.
Such a scenario leads to the next significant difference: non alcoholic fatty liver vs alcoholic fatty liver. In general, both diseases affect the same organ and have some similarities in symptoms. However, their causes, course, and treatment vary greatly. Knowing these distinctions is of great importance, as your liver works silently all day and night to purify your blood, digest fats, and regulate the energy of the body.
What is Fatty Liver?
Fatty liver simply means there is excess fat stored in your liver cells. Generally, the liver has some fat, but when the fat is more than 5-10% of the liver weight, it is considered unusual.
There are two main types of fatty liver diseases:
-
Non alcoholic fatty liver (NAFLD): Fatty liver occurring in people who consume little to no alcohol.
-
Alcoholic Fatty Liver (AFLD): Fatty liver is mainly due to excessive alcohol intake.
|
Feature |
Non Alcoholic Fatty Liver (NAFLD) |
Alcoholic Fatty Liver (AFLD) |
|
Cause |
Poor diet, obesity, diabetes, high cholesterol, sedentary lifestyle |
Excessive alcohol consumption |
|
Common in |
Non-drinkers, diabetics, people with metabolic syndrome |
Regular/heavy drinkers |
|
Progression |
Can advance to Non-Alcoholic Steatohepatitis (NASH) → Fibrosis → Cirrhosis |
Can progress to Alcoholic Hepatitis → Fibrosis → Cirrhosis |
|
Symptoms |
Often silent; fatigue, mild discomfort, unexplained weight gain |
Fatigue, jaundice, nausea, abdominal pain |
|
Reversibility |
High, especially in early stages with lifestyle changes |
Possible if alcohol is stopped; worsens with continued drinking |
|
Risk Factors |
Obesity, type 2 diabetes, high triglycerides, poor diet |
Quantity, frequency, and duration of alcohol intake |
Bottom line: In the debate of non alcoholic fatty liver vs alcoholic fatty liver, organ damage may look similar, but the root causes and solutions vary.
Causes: Non Alcoholic Fatty Liver vs Alcoholic Fatty Liver
Non alcoholic fatty liver causes
-
Overeating calorie-dense foods (fried, sugary, packaged foods)
-
Insulin resistance and type 2 diabetes
-
High cholesterol and triglycerides
-
Sedentary lifestyle and lack of exercise
-
Hormonal imbalances, especially in women
Alcoholic fatty liver causes
-
Regular or heavy alcohol intake (over 20 g/day for women, 30 g/day for men)
-
Genetic predisposition (some livers break down alcohol slower than others)
-
Poor nutrition alongside drinking
-
Repeated binge drinking episodes
Symptoms to Watch For
Both conditions may remain silent for years, but when they show up, symptoms can include:
-
Unexplained fatigue and weakness
-
Dull pain or heaviness in the upper right abdomen
-
Sudden weight gain or difficulty losing weight
-
Jaundice (more common in alcoholic hepatitis)
-
Poor digestion and bloating
If ignored, both nonalcoholic fatty liver and alcoholic fatty liver can progress to serious stages like cirrhosis (scarring) or even liver cancer.
Treatments: How Are They Managed?
1. Lifestyle modifications
-
For non alcoholic fatty liver:
-
Weight loss (even a 7–10% reduction can help)
-
A plant-based, whole-food diet with less sugar and processed food
-
Regular exercise (at least 30 minutes of brisk walking, 5 days a week)
-
Controlling diabetes and cholesterol
-
For alcoholic fatty liver:
-
The patient must absolutely refrain from the consumption of any type of alcoholic beverage for an indefinite period of time.
-
Nutritional therapy (foods rich in proteins, vitamins, and minerals, fluids)
-
Counseling or recovery programs (if required)
2. Medical treatments
-
Doctors may prescribe medicines to control diabetes, cholesterol, or inflammation.
-
In alcoholic hepatitis, steroids or other drugs may be required.
3. Natural & nutritional support
Many studies highlight the role of natural compounds in supporting liver recovery:
-
Milk thistle (Silymarin): It is associated with less liver inflammation, and it also protects the liver from harmful substances. A clinical trial conducted in 2002 showed that there was a 30 - 41% improvement in liver enzymes (AST & ALT) when patients were treated with milk thistle in comparison with placebo.
-
NAC (N-Acetylcysteine): Rises glutathione (the body's main antioxidant) level to shield the liver cells from oxidative injury.
-
Kutki, Kalmegh & Bhumyamalaki: Support the regeneration of bile flow, balances enzymes, and facilitates the body's detox process.
These are particularly helpful in both non alcoholic fatty liver and alcoholic fatty liver, where oxidative stress and inflammation are key drivers of damage.
The Indian Lifestyle Factor
In India, the challenge is double-sided:
-
A huge population consumes alcohol socially or heavily, contributing to alcoholic liver disease.
-
At the same time, rising rates of diabetes, obesity, and junk food intake are driving nonalcoholic fatty liver.
That means whether or not you drink, your liver is under constant stress from pollution, processed food, stress, and medicines.
Can Fatty Liver Be Reversed?
Yes, especially in early stages. Both nonalcoholic fatty liver and alcoholic fatty liver can be managed or even reversed if detected early and treated with the right lifestyle, medical, and nutritional interventions.
The key is early diagnosis and consistent care. Don’t wait for symptoms; if you’re overweight, diabetic, or a regular drinker, get a simple liver function test (LFT) done.
A Smarter Way to Support Your Liver
While lifestyle remains the foundation, modern science shows that certain natural compounds can speed up liver healing. That’s why some people add plant-based liver detox supplements to their routine.
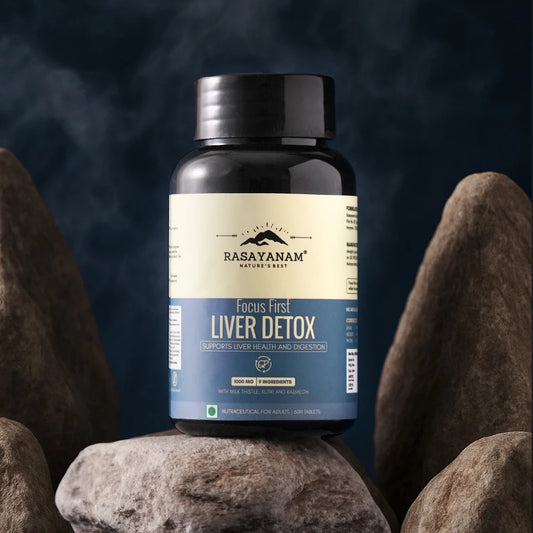
For example, Rasayanam Focus First Liver Detox offers comprehensive 360° liver support through a unique blend of 9 powerful ingredients, including clinically proven Milk Thistle (80% Silymarin – 400 mg) and NAC (120 mg), along with 3 traditional liver-supporting herbs like Kutki, Kalmegh, and Bhumyamalaki, 2 antioxidants like Dandelion & Turmeric, and 2 essential minerals like Zinc & Selenium. This powerful blend is crafted to help with both prevention and recovery, making it perfect for daily detoxing and promoting liver health. Together, they:
-
Detoxify the liver from alcohol, junk food, medicines, and pollutants
-
Restore liver enzymes (AST, ALT, GGT) naturally
-
Improve digestion and fat metabolism
-
Provide long-term antioxidant protection
-
Promotes recovery from fatty liver and soothes inflammation
Also Read: Why Timing is Everything While Taking Shilajit
Final Takeaway
The debate of non alcoholic fatty liver vs alcoholic fatty liver isn’t about which one is “worse”; it’s about realizing that both can silently harm your health if ignored.
-
If you don’t drink, you’re not automatically safe; watch your diet, weight, and activity.
-
If you do drink, remember that moderation or abstinence can make the difference between recovery and irreversible liver damage.
-
In both cases, your liver deserves daily protection, mindful habits, and natural support.
If you are looking for a little additional help, a gentle, natural support like Rasayanam first liver detox focus can give the daily care your liver needs.
Frequently Asked Questions:
1. Does everyone who drinks heavily get alcoholic fatty liver?
Not always. Genetics, diet, and overall health play a role. But studies show from (PMC) that a higher number of heavy drinkers will develop alcoholic fatty liver at some stage. The risk of progression to cirrhosis is much higher in long-term drinkers.
2. Which is more dangerous: non alcoholic fatty liver vs alcoholic fatty liver?
Both can be serious when untreated. Alcoholic fatty liver tends to deteriorate rapidly if alcohol use continues, while NAFLD is slow, but often goes unnoticed until it is advanced. The actual risk is ignoring the situation for a long time.
3. Do children or teenagers get non alcoholic fatty liver?
Unfortunately, yes, with rising junk food and screen time, non alcoholic fatty liver is being diagnosed in kids and teens. Early intervention through healthy eating and activity is key. Ignoring it in youth can lead to serious problems later.
4. What is alcoholic hepatitis?
It’s a severe stage of alcohol-related damage where the liver becomes inflamed. Unlike simple alcoholic fatty liver, this stage often causes jaundice, fever, and abdominal pain. Without treatment, alcoholic hepatitis can be life-threatening.
5. How long does it take for non alcoholic fatty liver to reverse?
With consistent lifestyle changes, NAFLD can start improving in 2-3 months. The timeline depends on weight, diet, and other health conditions. Supplements with liver-protective herbs may help speed up recovery.
6. Is fatty liver painful?
Most cases of non alcoholic fatty liver and alcoholic fatty liver are silent with no pain. Some people may feel heaviness or discomfort on the right side of the abdomen. Pain usually appears in more advanced stages like hepatitis or cirrhosis.
Disclaimer: This blog is for educational purposes only. It is not a substitute for medical advice, diagnosis, or treatment. Always consult your doctor before starting any supplement or making major lifestyle changes, especially if you have liver disease or are on medication.